Abstract
Adverse drug effects are common in clinical practice and often have a negative impact on patient safety. Heparin and heparin-derived drugs may induce an immune reaction, termed heparin-induced thrombocytopenia (HIT). HIT is mediated by IgG antibodies with specificity for heparin/platelet factor 4 (PF4) antigenic complexes. HIT is a hypercoagulable state which often causes severe and extensive thrombosis that results in high morbidity and mortality. The prevailing view is that these immune complexes activate platelets via FcγRIIa receptors leading to thrombocytopenia and thrombosis.
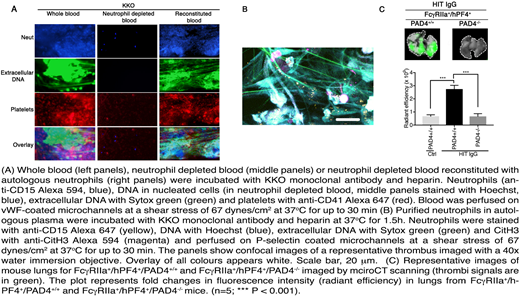
Neutrophil extracellular traps (NETs) are DNA-containing structures released by neutrophils that are increasingly being reported in patients with infection and thrombosis associated with various autoimmune and non-immune disorders. Here we show that HIT immune complexes directly activate neutrophils via FcγRIIa and induce NETs formation. In addition, NETosis is also induced by activated platelets/neutrophil interactions mediated by P-selecting and PSGL-1. Ex vivo reconstitution of the HIT condition in a microfluidics system demonstrated the formation of thrombi rich in platelets, neutrophils, extracellular DNA and citrullinated histone 3 (Figure 1A, left panels). Neutrophil depletion abolished thrombus formation. Conversely neutrophil reconstitution restored thrombus deposition (Figure 1A, middle panels and right panels). Moreover, neutrophils alone treated with HIT IgG plus heparin formed thrombi containing extracellular DNA networks and citrullinated histone 3 on P-selectin coated channels (Figure 1B).
Establishment of HIT in hFcγRIIa+/hPF4+ transgenic mice (HIT mice) using HIT patient's IgG or the HIT-like monoclonal antibody KKO recapitulated the hallmarks of NETosis: citrullinated histone 3, cell free DNA and MPO were detected in plasma and the presence of neutrophils, extracellular DNA and citrullinated histone 3 was found in lung thrombi. Low density neutrophils were also present in HIT mice treated with HIT IgG plus heparin but not in animals treated with control IgG. Treatment of HIT mice with DNase I or NETs formation inhibition with the PAD4 inhibitor GSK484 led to a dramatic decrease in thrombosis. This was corroborated by deletion of PAD4 in HIT mice. No thrombi were detected in hFcγRIIa+/hPF4+/PAD4-/- mice treated with HIT IgG and heparin (Figure 1C), indicating that NETs formation is required for thrombosis. Unlike thrombosis, thrombocytopenia was not affected by the absence of NETs formation, suggesting that these are separable processes. However, they are FcγRIIa-mediated mechanisms as anti-FcγRIIa antibodies abolished both processes. Analyses of sera from HIT patients revealed the presence of NETs markers and a significant proportion of neutrophils from patients with active HIT were undergoing NETosis. Our observations demonstrate that NETs formation is present in HIT and that it is essential for the development of thrombosis. Thrombocytopenia is not affected by the absence of NETosis. These findings suggest a new concept of the pathogenesis of thrombosis in HIT and as such are of clinical significance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal